Inflammation of the Pancreas in Dogs: Diagnosis and Treatment
a.k.a. Pancreatitis, inflammation of the pancreas

SUMMARY OF CONTENT
SEVERITY:
-
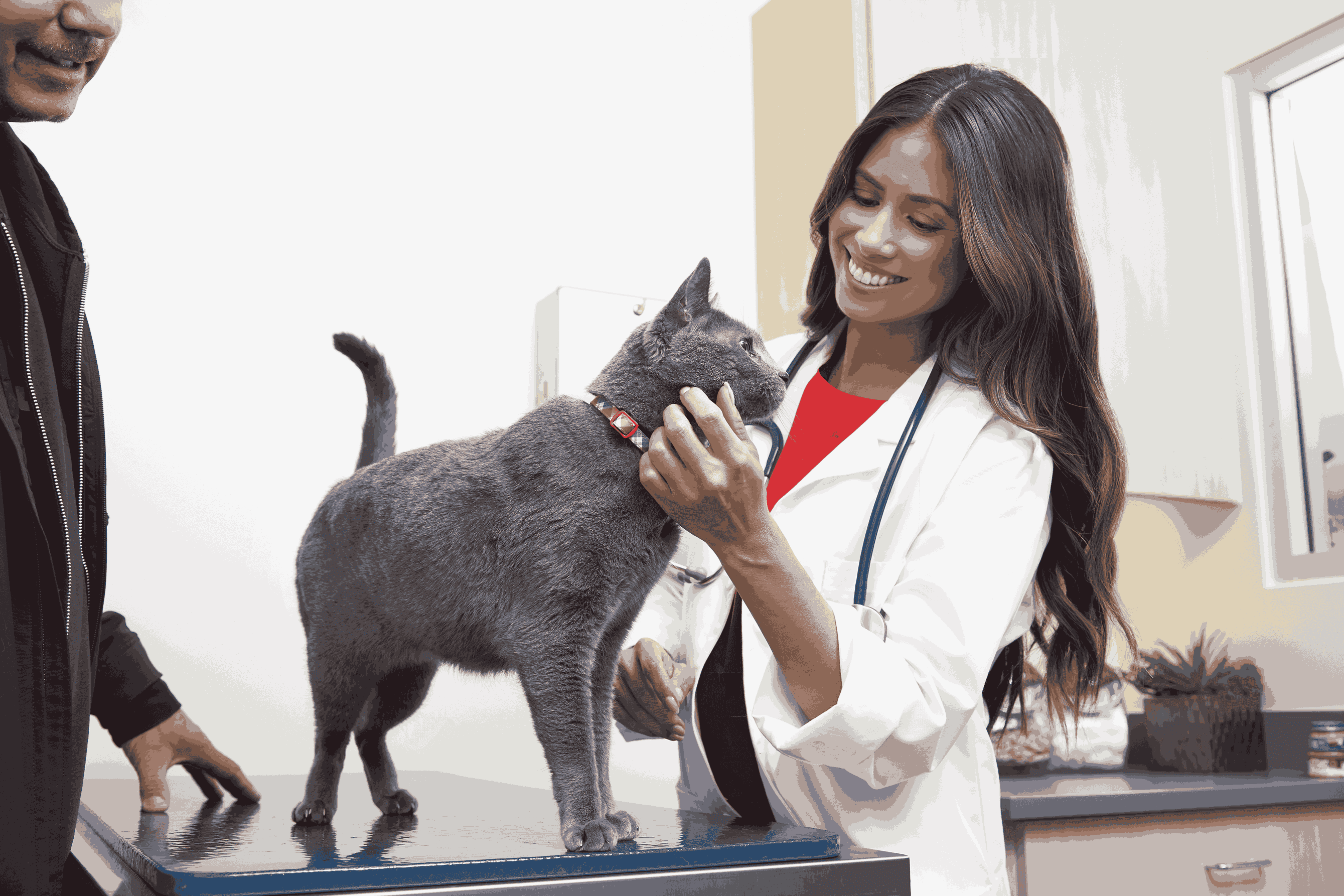
 Requires a diagnosis by a veterinarian
Requires a diagnosis by a veterinarian -
 Resolves within days to weeks, or is a chronic condition
Resolves within days to weeks, or is a chronic condition -
 Treatable by a veterinarian, by the pet parent
Treatable by a veterinarian, by the pet parent -
 Avoiding fatty foods and maintaining a healthy body weight are the best ways to try to prevent pancreatitis
Avoiding fatty foods and maintaining a healthy body weight are the best ways to try to prevent pancreatitis -
 Not contagious to other pets or people
Not contagious to other pets or people -
 Physical exam, lab tests, abdominal ultrasound, surgical biopsy (rare)
Physical exam, lab tests, abdominal ultrasound, surgical biopsy (rare)
VERY COMMON IN
Symptoms & Signs
Most dogs with pancreatitis experience vomiting, anorexia (not eating) and lethargy. Some dogs display signs of abdominal pain (posing in a “prayer position” with forelimbs and head down while the hind end is positioned upwards, hunched posture, crying out or whining when the abdomen is palpated), dehydration and diarrhea. All of the signs for pancreatitis are considered non-specific, as they occur in a large number of other conditions and can vary widely in severity. Severely ill dogs with pancreatitis can present with severe dehydration, ascites (fluid in the abdomen), tachycardia (elevated heart rate), icterus (yellow gums, skin, white parts of the eye) or signs of petechiation (red lesions on the skin from broken blood vessels). In severe cases, pancreatitis can progress to a life threatening systemic inflammation.
Diagnosis
There is no single test that is definitive for all cases of pancreatitis. The diagnosis is based upon compatible results of exam findings, lab tests, diagnostic imaging, and rarely, surgical pancreatic biopsy. Common exam findings include abdominal pain, a low-grade fever and dehydration in the presence of vomiting, anorexia and diarrhea. More severely ill dogs can display signs of shock, bleeding issues, or icterus. Necessary lab tests include a CBC (complete blood count to evaluate red and white blood cells and platelets), blood chemistry (to evaluate organ function, lipase and amylase) and urinalysis (to evaluate kidney function and look for signs of infection). In the past few years, more specific tests for pancreatitis have become available and include the cPLI and Spec cPL blood tests. If these tests results are normal, pancreatitis can be excluded as a possible diagnosis with a great deal of certainty. However, if the test results are abnormal, this indicates that pancreatitis should be highly suspected. The cPLI and Spec cPL tests do not provide a definitive diagnosis of pancreatitis and must be interpreted in light of all other findings. Abdominal ultrasound can indicate inflammation of the pancreas and other consistent changes in the abdomen. Again, this is not a definitive diagnostic test and serves to raise or lower suspicion of pancreatitis. Abdominal x-rays can indicate changes in some cases, such as decreased abdominal detail or the presence of fluid. A definitive diagnosis of pancreatitis can only be made by means of a surgical pancreatic biopsy. This procedure is only performed in very severe cases of pancreatitis that are not responding to therapy, because it poses a number of risks and complications.
Causation
The pancreas is a glandular organ that is located near the stomach and upper small intestine (duodenum). It is responsible for releasing digestive enzymes, which aid in breaking down food, as well as producing insulin, which is a hormone that causes glucose (sugar) to be utilized for energy at a cellular level. The exact cause of pancreatitis is not fully understood, but it is thought that when the pancreas’ digestive enzyme levels are altered, the pancreas begins to damage itself (autodigestion) and cause significant inflammation.
Pancreatic enzyme alteration is suspected to occur due to a variety of risk factors. These include: obesity, eating a high fat meal, administration of certain medications (potassium bromide, certain chemotherapeutic drugs, trimethoprim-sulfa antibiotics, phenobarbital, or exposure to organophosphate insecticides), trauma to the pancreas (i.e. being hit by a car), endocrine disorders (hypothyroidism, Cushing’s disease or diabetes mellitus), hyperlipidemia, or pancreatic tumors.
Some of the bigger clinical concerns with pancreatitis are related of the changes it causes with other organ systems in the body. The pancreatic inflammation can extend to the liver and cause inflammation of the bile duct going to the gallbladder. The enzyme abnormalities can destroy blood clotting factors, which can cause DIC (disseminated intravascular coagulation) or other bleeding disorders, which can progress to multiple organ dysfunction syndrome (MODS). Abscesses (infection) can develop in the pancreas and can lead to a septic (severely infected) abdomen.
Diabetes mellitus can occur if a significant portion of the pancreas has been damaged, because the pancreas also produces insulin, and the destruction of insulin-producing cells leads to diabetes.
Treatments
AT-HOME CARE
SUPPORTIVE CARE
MEDICATIONS
DEVICES
SURGERY
SPECIALISTS
Cost Of Treatment
$200 and $1,000+ per episode This will depend on the size of the dog, the severity of the condition and how many days of hospitalization/treatment are required.
Recovery
Recovery for mild cases of pancreatitis can take several days to a week. More moderate to severe cases of pancreatitis can take several weeks to achieve full resolution. Some of the most severe cases of pancreatitis do not recover due to organ dysfunction and DIC, and those dogs succumb to disease or are humanely euthanized.
Monitoring
During hospitalization, dogs are monitored for changes in clinical signs (vomiting, appetite, lethargy, diarrhea), blood values (chemistry panels, coagulation tests, electrolyte levels), blood pressure and fluid input/urine output. At home, monitoring a dog’s appetite, energy level and for the presence of any vomiting or diarrhea are crucial to identify the recurrence of pancreatitis. The frequency of recheck appointments is based upon the severity of each individual case, as well as the response to initial treatment.
Prevention
For a dog that has never had a case of pancreatitis, avoiding fatty foods and maintaining a healthy body weight are the best ways to try to prevent pancreatitis. If a dog has previously been diagnosed with pancreatitis, feeding a low-fat diet for the long term, avoiding any known individual risk factors (certain medications, for example) or table foods are the mainstay of preventing recurrence of pancreatitis.
Questions about Inflammation of the Pancreas
Two Easy Ways to Start Earning Rewards!
Become a member today!Members-only pricing and offers, personalized care notifications, Vital Care points back on every purchase and more!Become a credit card member today!
Earn 2X Pals Rewards points at Petco
when you use Petco Pay!APPLY NOWLearn More About Petco Pay Benefits