Preventing Transmission of Infectious Diseases in Small Animals
Developed with and approved by a qualified veterinarian.

Types of infectious diseases in small animals
Small animals can carry infectious organisms that can potentially cause zoonotic (transmittable to humans and other animals) diseases. Among these organisms are:
- Lymphotocytic choriomeningitisvirus (causing lymphocytic choriomeningitis)
- Salmonella bacteria (causing salmonellosis)
- Streptobacillus moniliformisbacteria (causing rat bite fever)
- Gastrointestinal parasites (such as tapeworms)
- Dermatophyte fungi (causing dermatophytosis or ringworm infection on hair and skin)
Overview of infectious diseases
Lymphocytic choriomeningitis virus (LCMV) can infect humans or pet rodents when they are exposed to contaminated urine, droppings, saliva or nesting material from wild rodents. Some pet rodents may carry LCMV and, if infected, may have long-term infection and shed virus into their droppings or saliva; often, infected rodents do not exhibit clinical symptoms. Rodents and people may be exposed to LCMV when it enters broken skin, the nose, eyes or mouth, or through a bite from an infected rodent. Most people who become infected with LCMV do not realize they are infected or have only mild flu-like symptoms.
Salmonella is a bacterium that can be acquired through contact with an infected animal’s fecal material or soiled bedding. Infected animals may carry this bacterium in their intestinal tract and not show any clinical signs of illness, or they may display general signs of illness, such as wetness around the tail region, diarrhea, decreased appetite and lethargy. Human infection can take place by not washing hands after having direct contact with an infected small animal or with the animal’s habitat, accessories or substrate. Symptoms of salmonella infection in humans include vomiting, diarrhea, fever, lethargy and stomach cramps. Salmonella is of greatest concern for children due to their Immature Immune systems and their tendency to put their fingers in their mouths.
Tapeworms, specifically Hymenolepis nana (also called Vampirolepis nana), are one of the most common gastrointestinal parasites found worldwide. Rodents infected with this tapeworm typically do not show any signs of illness; however, severe infections can cause weakness, weight loss and diarrhea in the infected rodent. Like salmonella bacteria, tapeworms are generally acquired through oral contact with a small animal’s fecal material or soiled bedding. Humans infected with tapeworms may not show any signs; however, with heavy infections, humans may have diarrhea, lethargy, abdominal pain, headache and decreased appetite.
Rat bite fever, which in the United States is caused by the bacterium Streptobacillus moniliformis, is an infection transmissible to people from rats. Rats are carriers of this bacteria and typically show no signs of illness; however, they can pass the bacteria on to people via bites or scratches or when humans accidentally ingest rat feces in contaminated food or water. Symptoms of infection in people usually occur 2–10 days after exposure to an infected rat or its droppings and include abrupt onset of chills and fever, vomiting, back and joint pain, headache and muscle pain. A knowledgeable physician can make a diagnosis of rat bite fever based on symptoms and testing for the specific strain of bacteria that causes RBF. The rat can be tested by your veterinarian to determine if it is infected with Streptobacillus moniliformis.
Ringworm infection (dermatophytosis) is not a parasitic worm at all but an infection of hair and skin with trichophyton or microsporum species of microscopic fungi. Animals and people are both susceptible to ringworm infection, but this disease appears differently in these two groups. It is called ringworm because in people, this fungal infection causes a characteristic itchy, scaly, ring-like, red skin rash. In animals, however, ringworm infection does not appear as a ring-like rash but instead as hair loss and dry, flaky, crusty skin. Guinea pigs, chinchillas, hamsters, gerbils, mice and rats with ringworm infection often have bald patches of dry, crusty, scaly skin around their eyes, nose and ears that can gradually spread to other parts of their bodies. Ringworm infection is highly contagious and can be transmitted from animal to animal or from animal to person through direct contact with an infected individual or through contact with items (such as bedding or other habitat items) contaminated with microscopic fungal spores. These spores are highly resistant to disinfection and can persist in dry environments for years until they develop into the infectious form of the fungus, called fungal hyphae. Following an individual’s exposure to ringworm fungus, signs typically develop within 14 days of contact. Diagnosis of ringworm infection is made in both people and animals by testing skin and hair samples for the presence of DNA from the fungus. Treatment in both people and animals is generally with a course of medication for several week—topical antifungal medication for mild cases or oral antifungal medication for more serious cases. Environmental cleanup and disinfection (of the infected animal’s habitat, bedding and all habitat items) is critical in treatment, as reinfection is common if any microscopic fungal spores are left behind. Young animals and people with immature immune systems are more susceptible to ringworm infection, and one-time infection does not confer resistance to reinfection.
Precautions to take when handling small animals:
- Always wash your hands thoroughly with soap and water after handling pet rodents or cleaning up their droppings, habitats or areas where they have been
- Always carry hand sanitizer or disinfectant with you if you are handling any rodents outside your home or in an area that lacks proper washing facilities
- If transporting a rodent to a classroom with children, make sure there are proper hand washing and cleaning facilities; do not take a rodent to a classroom or daycare facility where there are children under age 5, and if you do have a rodent in a classroom, do not allow children to touch the animal
- Keep your rodent habitat, water and food bowls, décor and other surfaces as clean as possible and free of soiled bedding
- Clean habitats in a well-ventilated area or outside
- Wear rubber, latex, vinyl or nitrile gloves when cleaning the habitat, and wash hands thoroughly when you are done
- Once the habitat is cleaned of organic material, disinfect it with pet-safe habitat cleaner, dilute bleach solution (a half-cup of bleach to one gallon of warm water) or disinfectant
- Let the habitat cleaner, bleach solution or disinfectant remain on the habitat and all food bowls, water dishes, hide huts, etc., for 10 minutes, then thoroughly rinse everything with warm water; allow everything to completely dry before returning your animal and their items to the habitat
- Make sure there is no lingering smell of cleaner, bleach or disinfectant, as small animals are very sensitive to chemicals
- Closely supervise young children when they are cleaning habitats or handling pet rodents, and ensure they wash their hands immediately after handling a pet rodent, habitat, accessories or bedding
- Children under five years of age should not help clean habitats or their contents, as they often put their hands into their mouths
- Do not handle your rodent or habitat furnishings with open sores or cuts on your hands because of increased risk of infection; wear rubber gloves to handle rodents and to clean habitats and habitat contents
- Never let your mouth contact your rodent; some people like to give their rodent an affectionate kiss, but kissing a rodent is not recommended, as this gesture can transmit infection to the person kissing the animal
- Pet rodents should be kept out of the kitchen and other food preparation areas
- Kitchen sinks and bathtubs should not be used to bathe rodents, clean habitats or wash rodent items; if you must use a sink or a tub, first remove all materials used to cook, prepare or serve food, and disinfect the area thoroughly with a mild bleach solution when finished
- Pet rodents should not be allowed to roam freely throughout the home or living area where they can pass potentially infectious droppings
- Persons at risk of infection or serious complications of zoonotic disease, children less than 5 years of age, immunocompromised persons, senior citizens and pregnant women or women trying to become pregnant should avoid contact with rodents
- Families expecting a new child should transfer the care of their pet rodent to a trusted family member, friend or neighbor prior to the infant’s arrival
- By following safe animal handling practices, you help ensure your safety and that of your animal
FAQs
- What are common diseases in small animals? Common diseases carried by small animals include rat bite fever, salmonellosis, lymphocytic choriomeningitis, tapeworm infection and ringworm infection.
- Can guinea pigs make you sick? Guinea pigs are rodents that can carry some illnesses that are transmitted through direct contact or through contact with infected droppings. These diseases are preventable by thoroughly washing your hands after handling guinea pigs, their droppings or items in their habitats.
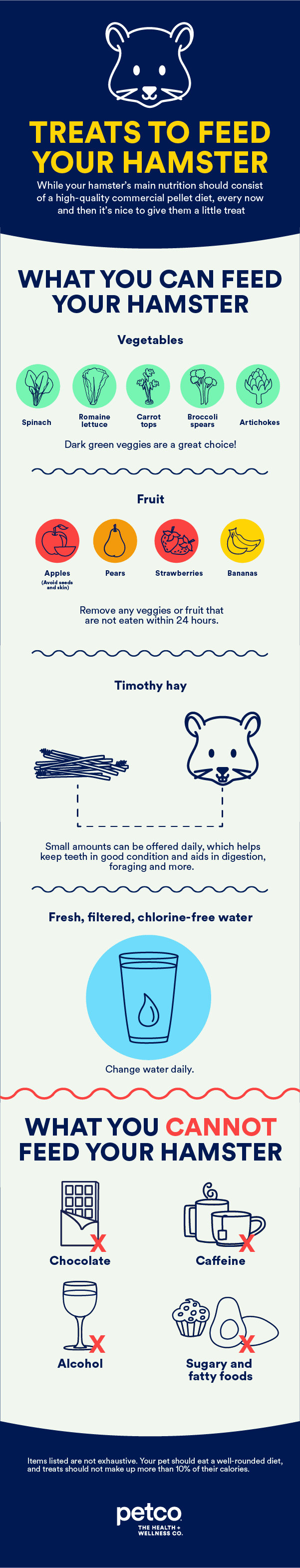
- What diseases do hamsters carry? Hamsters are rodents that can carry diseases such as lymphocytic choriomeningitis, salmonellosis, tapeworms, ringworm fungus and others.
Notes and resources
Because small animals are potential carriers of infectious diseases that can be transmitted to people, always wash your hands before and after handling your pet and/or habitat contents to help prevent the potential spread of disease. Work with your veterinarian on protocols to treat your pet and keep you and your family safe should your pet contract one of these diseases.
The information on this care sheet is not a substitute for veterinary care. If you need additional information, please contact your veterinarian as appropriate.
Related Articles
Related Questions
Sponsored
Two Easy Ways to Start Earning Rewards!
Become a member today!Members-only pricing and offers, personalized care notifications, Vital Care points back on every purchase and more!Become a credit card member today!
Earn 2X Pals Rewards points at Petco
when you use Petco Pay!APPLY NOWLearn More About Petco Pay Benefits